Breast Cancer – Essential Facts, Prevention, and Treatment Guide
Breast cancer is the most common cancer among women worldwide, but it’s not a death sentence. With early detection and modern treatments, many people live full, healthy lives after a diagnosis. This guide breaks down the key points you need to know, from warning signs to the latest treatment options.
Common Signs and Risk Factors
Knowing what to look for can help you spot a problem early. The most typical sign is a new lump in the breast or underarm. It might feel hard, uneven, or painless. Other changes to watch for include swelling, skin dimpling, nipple retraction, or unexplained discharge. If any of these appear, schedule a doctor’s appointment right away.
Risk factors are a mix of things you can’t change and things you can. Age is the biggest factor – the risk rises after 40. Family history also matters; having a close relative with breast cancer doubles your chances. Certain genetic mutations, like BRCA1 or BRCA2, increase risk dramatically. Hormone‑related factors such as early periods, late menopause, or hormone‑replacement therapy add to the odds. Lifestyle choices count too: maintaining a healthy weight, limiting alcohol, and staying active can lower risk.
Screening, Treatment, and Support
Screening saves lives by catching cancer before it spreads. In most countries, women start routine mammograms at age 40‑50 and continue every one to two years. If you have a strong family history or a genetic predisposition, your doctor may recommend earlier or more frequent scans, sometimes adding MRI for extra detail.
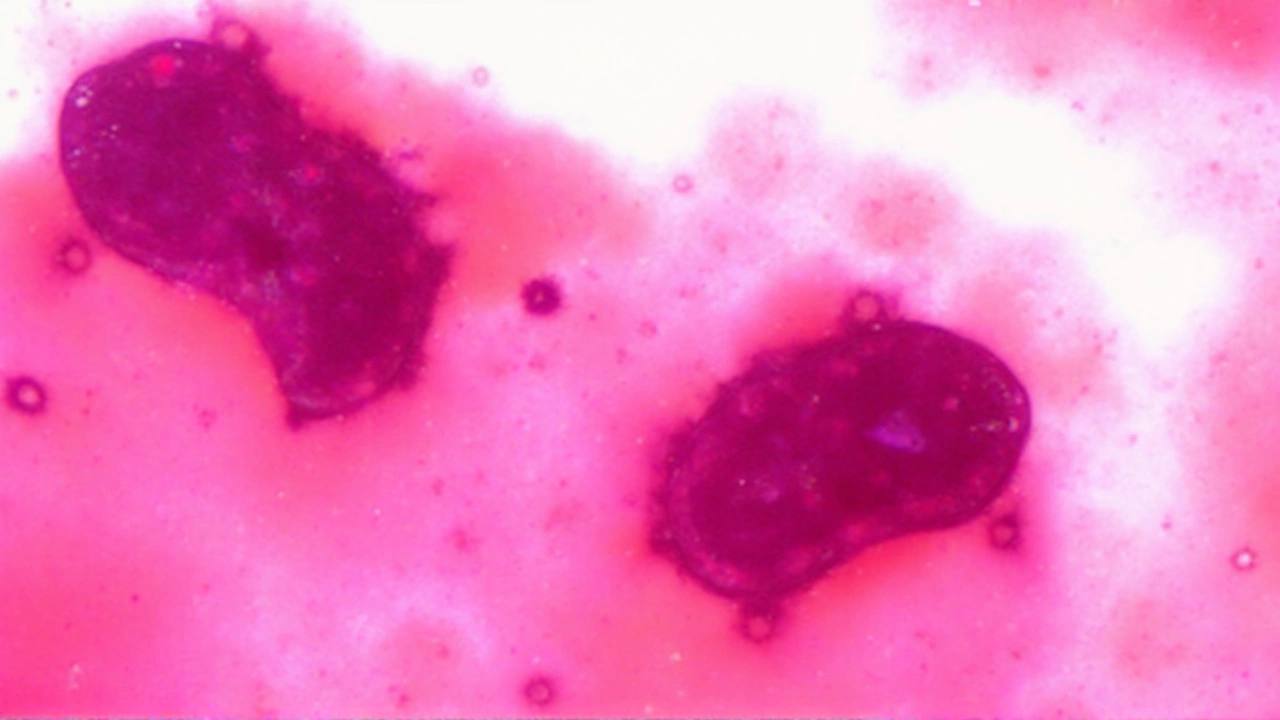
When cancer is found, treatment depends on size, stage, and hormone‑receptor status. Surgery is often the first step – either a lumpectomy (removing just the tumor) or a mastectomy (removing the whole breast). Radiation therapy follows many surgeries to kill any remaining cells.
Chemotherapy, hormone therapy, and targeted drugs are used when the cancer is more advanced or to lower the chance of recurrence. Hormone‑positive cancers respond well to drugs like tamoxifen or aromatase inhibitors. HER2‑positive tumors can be treated with trastuzumab and similar agents, which specifically attack that protein.
Support doesn’t end with medical care. Emotional and practical help is crucial. Many hospitals run support groups where patients share experiences. Counselors, nutritionists, and physiotherapists can address side‑effects, mental health, and physical recovery. Online communities also offer a place to ask questions and find encouragement.
Staying proactive is the best defense. Keep a regular self‑exam routine, attend scheduled screenings, and talk openly with your doctor about any concerns. If you’re at higher risk, ask about genetic testing and preventive options like medication or risk‑reducing surgery.
Remember, breast cancer is a journey that looks different for everyone. With the right information, early detection, and a solid support network, you can navigate it confidently and maintain a good quality of life.
Capivasertib: New Hope for Advanced Breast Cancer in Global Phase III Trial
The CAPItello-291 phase III trial explores capivasertib, an AKT inhibitor, in combination with fulvestrant for HR-positive, HER2-negative advanced breast cancer. Enrolling 830 patients worldwide, this trial aims to provide new treatment options for cases resistant to aromatase inhibitors. Developed by ICR, Astex, and AstraZeneca, this trial addresses urgent treatment gaps in metastatic breast cancer.
View more